BY BETTY MABERRY, JORDAN SMITH, AND ASHLEY TAPP
THE HELPDESK TEAM
Reminding employees of their current insurance coverage throughout the year is a valuable approach in showing your team their opportunities to be informed and encouraged to navigate benefits and coverage that you offer as an employer independently.
The Bottoms Group (TBG) has received positive feedback from various employers who communicate effectively with their staff when it comes to having detailed actions in place for members to be able to access their benefits efficiently. A successful method in reaching employees and motivating them to be confident and familiar with their coverage can be as simple as sending out a company-wide email including a bullet point format of easy-tofollow instructions on how to access online benefits. An employee may also be more inclined to take the initiative to register/login on an online carrier portal, if they receive a flier from the insurance carrier demonstrating the advantages in gaining access through the carrier’s member portal.
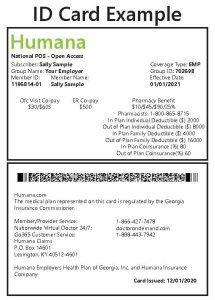
One of the first things an insurance carrier will do once an employee is enrolled, is generate a member I.D. number, and send out a member I.D. card. A member I.D. card is a beneficial tool that contains a plethora of helpful details such as the member I.D. and group I.D. numbers, a few coverage details for easy reference, phone numbers for Member and Provider Services, the carrier portal website, and contact information for Online Carrier Portal Support Services.
Once your employee has their member I.D. number, they will be able to register and login to the insurance carrier’s online portal. Registered employees can use the carrier’s website to download electronic I.D. cards, view coverage and claim details, evaluate Explanation of Benefits (EOBs), search for in-network providers and so much more. Additionally, many insurance carriers have a smart phone application which gives members the opportunity to have immediate access to their coverage. Registering and logging into the carrier portals allows enrolled employees to take full advantage of their new coverage.
In addition to using I.D. cards to register on the carrier portal, notifying their providers, pharmacies, and facilities of their updated member I.D. card details is a key factor in helping with claim submissions throughout the plan year. Your team should also be aware during the year to select providers that are participating and contracted with the insurance company prior to services rendered in order to maximize their current benefits with innetwork coverage. Recently, our TBG Help Desk team was notified by an employee whose claims were being denied because their provider did not have the employee’s updated insurance details. Although you can usually expect the provider to request updated insurance information before an appointment, it is highly suggested that employees proactively update their providers with their new coverage details, prior to services rendered. Ultimately in this situation, our TBG Help Desk was able to assist by contacting the provider, as well as the carrier, to have the claims reprocessed accordingly.
Using the member I.D. card, enrolled employees can take charge of their coverage and fully make the most of all their plan has to offer. As always, our TBG Help Desk team stands ready to assist your employees should they have questions about how their claims processed, or with anything else that may arise.


